Worldwide, penile cancer is a serious health issue. Trans individuals are a vital demographic that is frequently disregarded, despite the fact that the majority of discussions and studies concentrate on cisgender men. Recently, Drs. Sandhya Srinivas and @AriaOlumiMD highlighted the obstacles and options for transgender people’s prostate cancer screening, treatment, and care. In the context of malignancy diagnosis and treatment, their conversation emphasizes the importance of healthcare professionals being aware of and sensitive to the particular needs and experiences of transgender people.
Recognizing the Special Needs of Transgender Patients
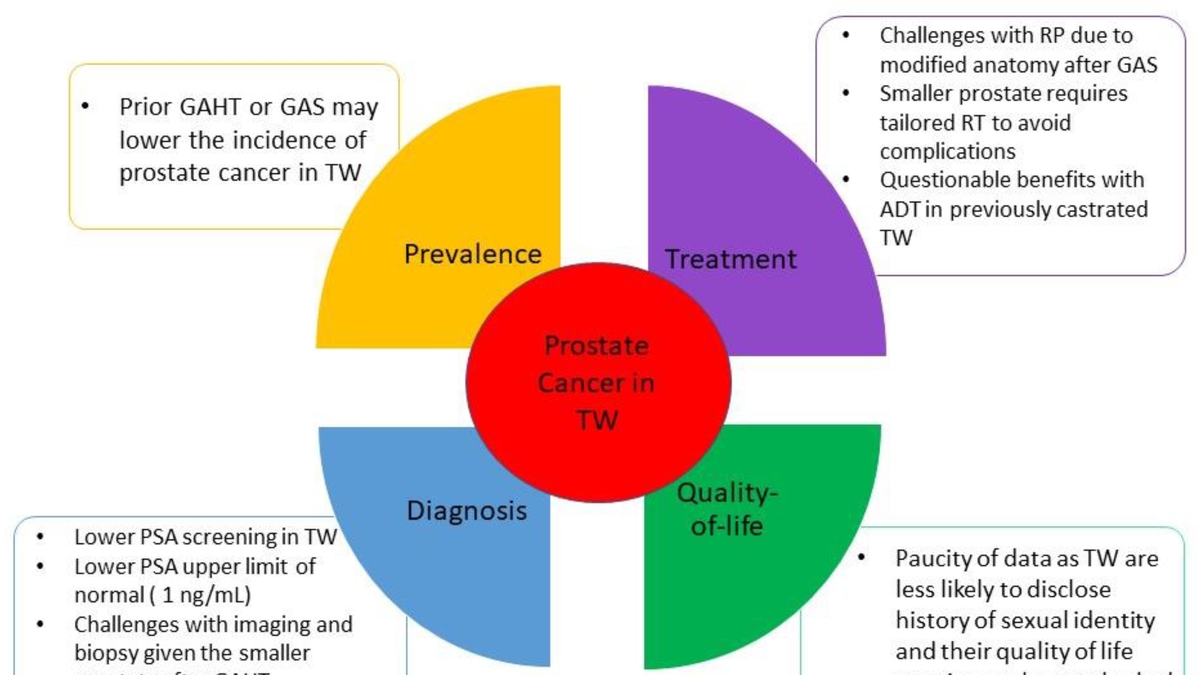
Trans people have special and intricate healthcare needs, particularly in the case of prostate cancer. For instance, transgender women may still have a prostate gland despite having gender-affirming surgery, increasing their risk of developing prostate cancer. There may be major obstacles to the successful monitoring and early diagnosis of prostate cancer for these individuals due to healthcare providers’ ignorance, knowledge, and sensitivity.
Obstacles to Screening and Treatment for Prostate Cancer
Successful prostate cancer screening and care for transgender people is hampered by a number of obstacles. These include lengthy wait times, a lack of understanding of transgender health issues among healthcare professionals, low patient health literacy, and difficulties in patient-provider communication. Trans people may also be unable to access timely and suitable medical care due to societal stigma and discrimination.
Putting a Strong Emphasis on Shared Decision-Making
It takes a patient-centered approach to overcome these difficulties. Shared decision-making (SDM) has the potential to greatly increase patient knowledge and lessen decisional conflict. Requirements for SDM facilitators include a regular clinician-provider relationship, confidence in the physician, having a partner, and having advanced education. Despite its advantages, SDM is still underutilized, primarily because of the aforementioned obstacles. Implementing decision aids can help SDM and increase patients’ knowledge.
The Need for Gender-Affirming Treatment
There is an urgent need for gender-affirming, wraparound care, as Drs. Srinivas and Olumi’s conversation highlights. This strategy fosters respect and a climate where patients feel at ease discussing their health concerns by respecting and affirming the patient’s gender identity. Gender-affirming care can drastically improve the standard of care given to transgender patients, resulting in better health outcomes.
Conclusion
The discussion between Drs. Srinivas and Olumi sheds light on the complexities of transgender medical care and the significance of gender-affirming care in oncology. Healthcare professionals must comprehend and target the particular needs of trans people in the framework of prostate cancer. By doing this, we can progress toward a medical system that is more inclusive, diverse, and effective.



