Most transgender people in the US who take hormone drugs do not suffer serious side effects – but for those who do, the symptoms are usually life-threatening.
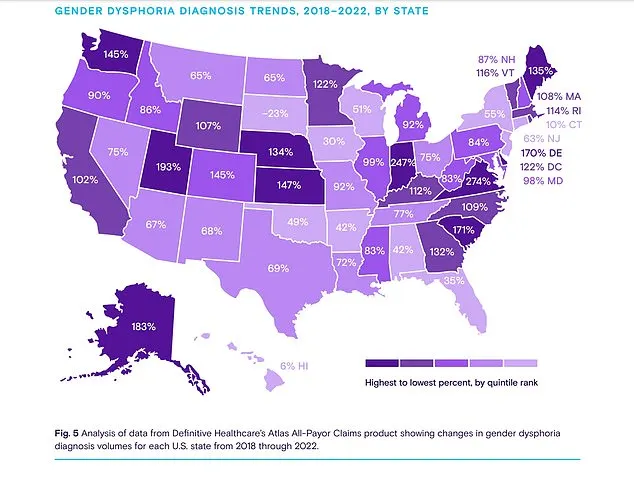
That is the conclusion of one of the first studies on the therapies, which have been increasingly used off-label in recent years to treat gender dysphoria.
The researchers analyzed the FDA’s Adverse Event Reporting System (FAERS) for side effects that occurred in trans people taking the medications to affirm their new gender.
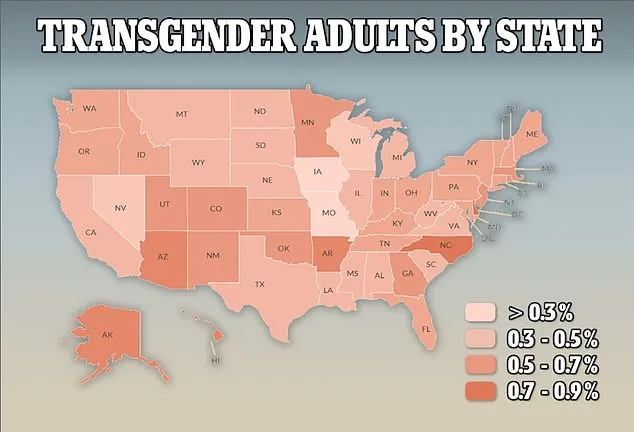
They found just over 400 cases of adverse side effects, dating as far back as the database goes until June 2023. However, given that at least 700,000 trans Americans are estimated to be on the drugs, the researchers said the true number of adverse reactions is likely ‘underreported.’
Of the reports, up to 88 percent were the most serious type – including organ damage, cancer, and death. The study team described this high number of serious events as ‘striking.’
The researchers – from Georgia and Utah – said their findings ‘should be interpreted cautiously’ because FAERS reports are voluntary and anyone can log one – including patients, family members, healthcare providers and vaccine manufacturers.
The reports are also not verified, which means the medication did not necessarily cause the reaction listed, just that they are believed by the patient or doctor to be linked.
However, by the same token, the researchers said ‘the voluntary nature of these reports may lead to underreporting, thus potentially underestimating the actual incidence of adverse events.’
The FAERS system is meant to act like an early warning system for side-effects. Data must be carefully analyzed, however, to determine whether any patterns are caused by the drug or are from another factor.
The latest analysis by pharmacists from the University of Utah and the University of Georgia is the first of its kind.
In it, they examined 467 adverse drug reactions.
The average age of trans men (female at birth and transitioning to male) was 29.5 years while the average age of trans women was 33.3 years.
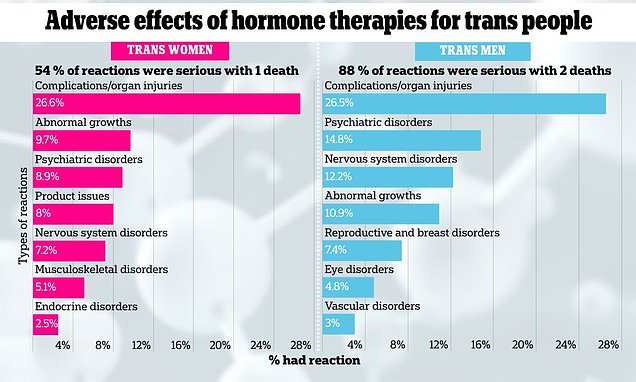
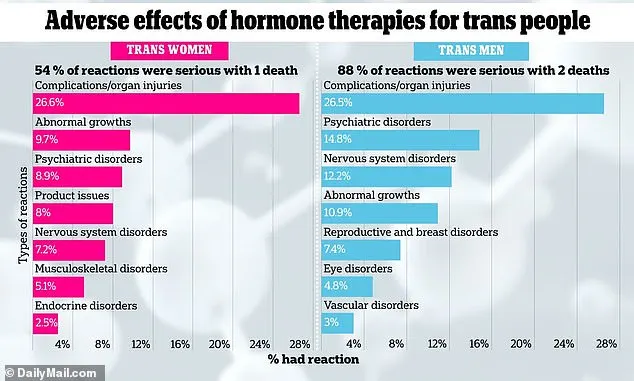
Of those adverse events reported in trans men, 88 percent were categorized as serious, while the figure was 54 percent for trans women.
Most of these injuries reported in trans men – 26.5 percent – were injuries to organ systems, poisoning, and complications such as infections, bleeding at the injection site, and nerve damage.
Psychiatric disorders accounted for 14.8 percent of adverse events in trans men, and nervous system disorders accounted for 12.2 percent.
In the group of health issues related to injuries, poisonings, and procedure complications, the most common problem reported was ‘off label use of the product’ (44 cases, or about 72.1 percent of all), though the researchers did not specify whether that meant people were taking the wrong doses or taking the medicines too often or too infrequently.
In terms of mental health problems, people reported feeling anxious (11.8 percent), depressed (8.8 percent), or having thoughts of suicide (8.8 percent).
Among issues with the nervous system, a condition called idiopathic intracranial hypertension – a rare neurological condition characterized by increased pressure within the skull – was the most frequently reported (18 cases, or about 64.3 percent).
About 11 percent of reported problems were related to growths in the body, with breast cancer being the most common (12 cases, or about 48 percent).
While this is not to say supplementary estrogen was the cause of people’s breast cancer, studies have shown that higher blood levels of the estrogen called estradiol are linked to an increased risk of breast cancer in postmenopausal women.
In the category of problems related to the reproductive system and breasts, there were 17 cases reported, making up about 7.4 percent of all.
In trans women (male at birth transitioning to female), a significant number of adverse events (63 cases, which is around 26.6 percent) were related to issues like injuries, poisonings, or complications from medical procedures.
The most common specific problem in this category was using drugs in a way not officially approved (40 reports, making up about 63.5 percent).
About 11 percent of the ADRs were grouped under general disorders and conditions related to where the medication was administered.
Additionally, almost 10 percent of the reports fell into the category of growths in the body (benign, malignant, and unspecified), with mentions of meningioma and prolactin-producing pituitary tumors being the most frequent.
Nearly nine percent of adverse reactions were mental health disorders, including two cases of anxiety, seven cases of depression, one case of insomnia, and one suicide attempt.
Among nervous system issues, headache was the most common with three cases. Some other issues included dizziness, attention disturbances, migraine, stroke, and aphasia, all of which had just one case.
Modern hormone therapies were first designed in the early-20th century to alleviate symptoms of menopause, such as hot flashes and vaginal dryness, by supplementing declining hormone levels in women.
But in recent decades, they have been prescribed off-label to people experiencing gender dysphoria, or a sense of distress due to the mismatch between the sex they were born into and the gender with which they most closely identify.
Still, there have not been comprehensive studies into the long-term safety effects of these drugs in that patient group, and many neuroscientists and reproductive health experts have raised questions about adverse effects and their safety when taken for long periods of time.

Hormone therapies can have a range of whole-body, system-wide effects that fall under this wide umbrella.
Introducing synthetic hormones or altering natural hormone levels can affect these systems, leading to adverse events such as electrolyte imbalances, cardiovascular complications, and immune-related reactions.
For instance, some hormone therapies may increase the risk of heart complications such as high blood pressure, blood clots, or arrhythmias.
They could also potentially lead to irritation in the digestive tract, resulting in bleeding or holes in the intestines.
And problems with the way the drugs are administered, such as flaws in injections, can lead to infections, tissue damage, or improper dosing.
In the case of events regarding trans men, 88 percent were logged by a healthcare professional, while 12 percent were logged by the patient.
In instances of reports regarding trans women, 67 percent of reporters were healthcare professionals while around 30 percent were from patient or a loved one.
Hormone therapies are meant to endow trans people with the secondary sex characteristics of their gender identity.
For transgender women, hormone therapy typically involves the administration of estrogen and anti-androgen medications, which suppress the effects of testosterone and induce feminizing changes such as breast development, redistribution of body fat, reduction in body hair, and softening of the skin.
For trans men, hormone therapy typically involves the administration of testosterone.
Testosterone promotes masculinizing changes like deepening of the voice, increasing muscle mass and strength, growing facial and body hair, and redistributing body fat.
But the medicines come with considerable health risks, including those reported to the FDA.
The researchers said while these treatments have helped thousands of gender dysphoric patients, they are prescribed off label and their safety risks should never be understated.
They wrote: ‘It is imperative that the therapeutic objectives for patients considering HT are clearly defined before commencing treatment.
‘This underlines the essential need for thorough knowledge and understanding for both patients and their health care providers.’
Experts from Mercy Catholic Medical Center in Darby, Pennsylvania, have found trans patients who take the drugs are up to seven times more likely to suffer an ischemic stroke compared to trans patients who are not prescribed them.
They were also nearly six times more likely to suffer myocardial infarction – the most serious type of heart attack – and had a five times higher risk of pulmonary embolism, a blockage in an artery in the lung.
Both estrogen and testosterone are known to increase blood clotting activity, which could explain the increased risk.
Hormone therapies are also known to make major changes in trans people’s emotional states. People taking estrogen, for instance, may cry more than they’re used to and even feel a greater sense of empathy. Some people may experience mood swings or a worsening of anxiety, depression, or other mental health conditions.
However a vast body of evidence has also shown that opening the door to gender-affirming care generally leads to improved quality of life, decreased depression, and reduced anxiety.
The findings were published in the journal Annals of Pharmcotherapy.



