When Cameron Whitley was diagnosed with kidney failure seven years ago, the news came as a shock. But the situation was about to get worse. His doctor decided the diagnosis meant Whitley’s hormone therapy had to stop.
As a transgender man, now 42, who had taken testosterone for 10 years, the impact was brutal.
“Not only was I struggling with this new diagnosis that I’m in stage four kidney failure, now I’m being told that I can no longer have hormones,” said Whitley, an associate professor in the department of sociology at Western Washington University. “I cannot describe how horrible that moment was.”
Crucially, he says, the decision was completely unnecessary. “We call this within the medical community ‘trans broken arm syndrome’,” he said.

The term refers to medical situations – such as having a broken arm – that are unconnected to gender identity, yet healthcare providers act on the basis there is a connection.
“We didn’t have any established sense that being on hormones would be problematic. The hormones are not processed through the kidneys. So there was nothing that made it [necessary to stop them], but that was the first thing that was done,” he said.
Whitely has since transferred his care over to the University of Pennsylvania, which he described as “awesome [with] wonderful trans-competent care”.
An increase in the number of people coming out as transgender has led to growing use of hormone therapies, which help to change the body’s physical characteristics towards a certain gender.
But as Whitley found out, misunderstandings and knowledge gaps about their impact abound.
While hormone therapies are today best known for their use in contraception or to manage symptoms of menopause in cisgender women, they have for decades been given to people undergoing gender reassignment. The German doctor Magnus Hirschfeld was one of the first to offer such medications to his patients at his Institute for Sexual Research in Berlin, which he opened in 1919.
Many people who are trans say such “cross-sex” or “gender affirming” hormone therapies are crucial: allowing them to live in a way that makes them happy and significantly reducing the risk of depression and suicide.
However, their use in younger people with gender dysphoria is controversial, not least because of their potential impact on fertility and the irreversible changes they can produce.
Until recently, gender-affirming hormone therapies in England could be given on the NHS after the age of 16, and individuals must have been on drugs known as puberty blockers for at least a year.
Puberty blockers pause the physical changes associated with adolescence, but have themselves been a key focus of concern when it comes to the medical treatment of children with gender dysphoria due to questions about their safety and clinical effectiveness.
New rules released by NHS England this month mean puberty blockers will no longer be used in treatments for under-18s with gender dysphoria, except as part of a clinical trial. A spokesperson for NHS England said amendments to the cross-sex hormones policy are being finalised in light of the new rules.
But away from the public debate about who should have hormone therapies and when, growing numbers of researchers are beginning to delve into their impact on the body in a bid to improve healthcare for trans people – and for the wider population.
For trans men, hormone therapy typically involves taking testosterone – enabling the growth of facial hair and a deepening of the voice, amid other changes – while for trans women it typically means taking oestradiol, which promotes the growth of breasts and an increase in body fat.
While such medications are known to change external appearances, how they might affect other aspects of the body – from the way internal organs work, to blood pressure and even risk factors for diseases – has been unclear. And that isn’t just true for trans patients.
“Regardless of the type of [hormone] therapy and who is using it, we actually surprisingly as a healthcare profession don’t know much,” said Dr Sofia Ahmed of the University of Alberta, who is looking at the impact of hormone therapy on kidney and cardiovascular health in transgender people.

“In using hormonal contraception, for example, we know it prevents pregnancy, but we have a limited understanding of how it affects kidney function, blood pressure, cardiovascular health – and that holds true for truly any kind of hormone therapy.”
For trans people taking hormone therapies, medics have raised particular concerns over standard “healthy” ranges for metrics such as blood pressure, kidney filtration rates or liver function.
These ranges are known to differ between cisgender men and women, but it is unclear what a “healthy” range is for trans men and women taking hormones – a situation doctors have said could put trans patients at risk of receiving the wrong dose of a medication, diseases being missed or even conditions being erroneously diagnosed.
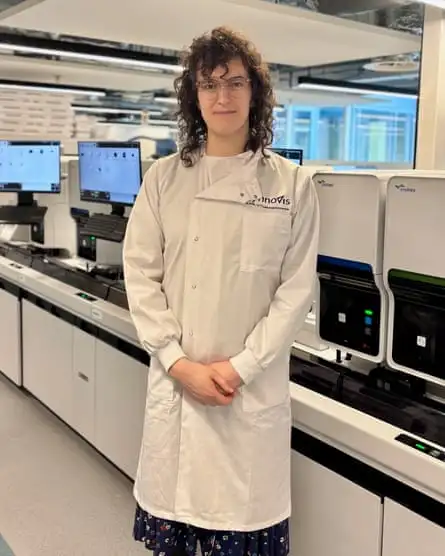
Among those attempting to resolve the issue is Dr Devon Buchanan, a clinical scientist with Synnovis who is running a trial based at King’s College hospital that began in April 2021 and is recruiting 240 trans and non-binary people.
“We know that those ‘normal’ ranges are affected by gender affirming hormone therapy which a lot of trans people take and is very important to them,” she said.
Many previous studies have been small and the results unclear. “We wanted to cover a wide variety of tests and also have a larger sample size so that we could be more sure about the results,” said Buchanan.
Studies have also suggested rates of obesity in trans people are higher than among those who are cisgender, but the reason for such disparities is unclear. Dr Sascha Heinitz of the University of Leipzig is examining the effects of hormone therapy on eating behaviour, metabolism, energy balance and the cardiovascular system in transgender people.
He and colleagues are following 20 trans men and 20 trans women, and the same number of cisgender participants, over a two- to five-year period.
“We [are] just trying to understand [whether], during gender affirming hormone therapy, [are] there any changes going on that increase the risk of developing these diseases,” he said.
Even if evidence points to a greater metabolic risk in individuals receiving hormone therapy, as some research has suggested, further work will be needed to explore the extent to which that could be down to physiological response of the body to therapy, changes to experiences of gender dysphoria, or behavioural changes around consumption of food, Heinitz noted.
Also in Germany, Dr Sofia Forslund-Startceva of the Max Delbruck Center in Berlin and colleagues are running a clinical trial with 200 transgender people to explore whether risk factors for cardiovascular disease relating to changes in the makeup of the gut microbiome that are known in cis men and women emerge as trans men and women take hormone therapy.
“In so doing, we can both learn more about the mechanisms underlying health disparities between cis men and cis women, and learn more on when and where and after how long in transition a trans person [is] better treated as someone of their reassigned sex as of their birth assigned sex,” she said.
Such research could also help to achieve personalised medicine by offering insights into the relationship between health and changing levels of various hormones.
For example, risk factors for various diseases are known to increase among post menopausal cisgender women, who have lower oestrogen levels and higher levels of hormones known as FSH and LH compared with those who are younger.
“Where I would like to see this going, both in cisgender medicine, in intersex care and in trans care, is perhaps to recognise the importance of sex and gender in medicine and healthcare,” she said, adding “maleness” and “femaleness” can exist in individuals to different degrees.
In other words, given levels of sex hormones can undergo a profound shift across an individual’s lifespan, whether cisgender or transgender, understanding their impact could have important implications for everyone’s healthcare.
Work in transgender health is still a relatively new field, and funding can be a struggle, as can recruiting a meaningful number of participants who are representative of the community.
And research does not occur in a vacuum: around the world transgender issues are a hot political and social topic, whether it’s the age at which individuals can access hormone therapy or who can use single-sex spaces.
“It is my experience, also from my outpatient clinic, that there is not only lack of knowledge, but also lack of interest, and also people who do not want to treat transgender individuals,” said Heinitz. “I think some people just don’t want to touch the topic because it’s too hot.”

Forslund-Startceva said her impression was not that the topic was avoided out of any fear of controversy. “That said, there may be a reluctance at least on the part of some [who see themselves as trans allies] to approach it since they fear as outsiders to the demographic that they would not be able to research accountably,” she said.
Some advocate the “nothing about us without us” approach, stressing teams without transgender members risk misunderstanding the community they are seeking to work with, could end up failing to ask the best questions to inform their research, and might run into problems when it comes to communicating results in a nuanced and comprehensive way.
“[The latter] matters when research becomes weaponised so quickly, because people will latch on to potential interpretations and misinterpretations and use them one way or the other as culture war tools that can do a lot of damage,” said Forslund-Startceva.
But the value of lived experience among researchers is contested. “You cannot bring anything personal into [the research] except for inter-individual contact, being friendly and nice,” said Heinitz.
“To have transgender individuals in this field is great. Not to have them would be not so good. But I mean, it’s not important to have subjects with kidney disease conducting a study on kidney disease.”
Despite the challenges, scientists say the possibilities of the new wave of research into hormone therapies is exciting, offering the chance to fundamentally change healthcare for the transgender community and more widely. “It has multiple layers,” said Heinitz. “It’s a beautiful field, I think.”
Forslund-Startceva agreed. “We start in the understanding that health and disease risks and responses differ between cis men and cis women, but one cannot easily entangle different components of sex or gender – is it due to lifestyle, hormones or genetics?”